In a 2023 article published in Heliyon and accessible via PubMed Central, a team of researchers led by Nathalie Möckli delves into the complexities of home healthcare coordination. Their work addresses a critical issue in healthcare: the lack of a clear and consistent framework for coordinating care, especially in home settings where multiple providers and tasks must be synchronized. This article introduces a comprehensive theoretical framework designed to clarify and streamline the concept of homecare coordination, offering valuable insights for researchers and healthcare professionals alike.
Home healthcare coordination is an increasingly critical component of modern healthcare, particularly as the population ages and the number of patients with chronic conditions rises. Effective coordination is essential to ensure that care is not only timely and efficient but also tailored to meet the individual needs of patients. Despite its importance, the concept of care coordination, especially within the home healthcare setting, remains somewhat nebulous, with varying definitions and a lack of clear measurement tools. This ambiguity can hinder research efforts and the implementation of effective coordination strategies.
To address these challenges, a recent article by Möckli et al. presents a comprehensive theoretical framework that aims to clarify the concept of home healthcare coordination. The framework distinguishes between coordination as a process and coordination as an outcome, providing a clearer understanding that could guide both future research and practical application.
Understanding Coordination in Home Healthcare
Home healthcare involves multiple participants, including healthcare providers, patients, and their families, all of whom must work together to deliver comprehensive care. This complexity makes coordination essential, but also challenging. Effective coordination must manage dependencies among various tasks and participants to avoid errors, inefficiencies, and unnecessary treatments that could negatively impact patient outcomes.
The framework proposed by Möckli et al. emphasizes the importance of distinguishing between coordination processes (the actions taken to coordinate care) and coordination outcomes (the degree to which these efforts result in seamless and effective care). This distinction is crucial because it allows for more accurate measurement and analysis of coordination efforts, avoiding the common pitfall of conflating the processes with their results.
Key Elements of the Theoretical Framework
The proposed framework is built on a thorough review of existing literature and integrates concepts from various theories of coordination. It introduces several key elements:
Coordination Mechanisms: These are the tools and methods used to manage dependencies between tasks. The framework distinguishes between explicit mechanisms, such as schedules and protocols, and implicit mechanisms, such as shared mental models and trust among team members.
Coordination Process: This refers to the actual implementation of coordination mechanisms. It includes both planned actions (like team meetings) and spontaneous adjustments made in response to emerging needs.
Coordination Outcomes: The framework highlights the importance of measuring coordination not just by patient outcomes (like recovery rates) but also by the effectiveness of the coordination itself. This means assessing how well tasks were managed and whether all necessary steps were taken without unnecessary delays or errors.
Influencing Factors: The framework also considers external factors that can impact coordination, such as organizational culture, the complexity of the tasks involved, and the broader healthcare environment. These factors can either facilitate or hinder effective coordination.
Applications of the Framework
One of the most significant contributions of this framework is its potential for standardizing the way coordination is understood and measured across different healthcare settings. By providing a clear and comprehensive definition of coordination, this framework can help researchers design studies that are more consistent and comparable. It also offers practical guidance for healthcare providers looking to improve their coordination efforts, particularly in the context of home healthcare.
For example, the framework can be used to identify gaps in current coordination processes and to develop targeted interventions that address these gaps. By focusing on both the processes and outcomes of coordination, healthcare teams can ensure that their efforts lead to meaningful improvements in patient care.
Conclusion
The theoretical framework developed by Möckli et al. represents a significant step forward in the field of healthcare coordination. By clarifying the concept of coordination and providing a structured approach to its measurement, this framework can guide both research and practice, leading to better outcomes for patients and more efficient use of healthcare resources. As the healthcare landscape continues to evolve, tools like this framework will be essential for ensuring that care coordination remains a priority in all settings, particularly in the increasingly important area of home healthcare.
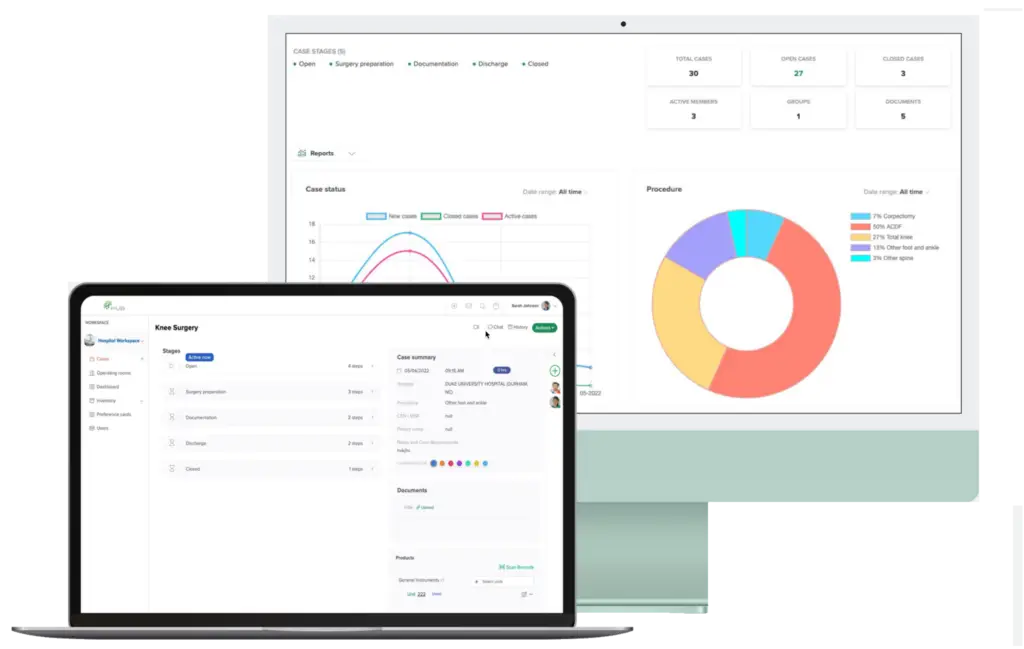
How HUB Healthcare Can Help
HUB Healthcare offers a comprehensive solution designed to enhance communication in healthcare, streamline care coordination, and improve overall workflow efficiency. Our platform includes features such as medical case management software, healthcare document management, and healthcare analytics to ensure that all aspects of patient care are optimized. By leveraging HUB Healthcare’s robust tools, organizations can reduce workflow bottlenecks, automate repetitive tasks, and facilitate better collaboration among healthcare providers. This not only improves work quality but also enhances patient outcomes, making HUB Healthcare an essential partner in achieving healthcare excellence.