Reimbursement delays are a persistent challenge for Ambulatory Surgery Centers (ASCs), straining both cash flow and long-term financial stability. These delays occur when claims are denied, rejected, or need manual intervention, creating bottlenecks in the revenue cycle and leaving ASCs vulnerable to cash flow problems. To overcome this, ASC leaders are increasingly shifting their focus to boosting first pass acceptance rates—the percentage of claims accepted on the first submission without requiring resubmission or correction.
This small but significant shift in focus can dramatically improve financial health by reducing denials and speeding up reimbursements. Let’s explore how ASCs can improve first pass acceptance rates, streamline claims management, and ultimately enhance both financial stability and the patient experience.

The Impact of Reimbursement Delays on ASCs
Reimbursement delays create a ripple effect on an ASC’s operations. When payments are delayed:
- Cash flow becomes strained, making it difficult to cover operational expenses.
- Manual labor increases, as staff must spend valuable time correcting claims.
- Patient satisfaction declines, since delayed payments may lead to billing confusion or extended payment timelines for patients.
Moreover, with the ongoing pressures of value-based care models and declining reimbursement rates, ASCs are often operating on razor-thin margins. For many centers, even small delays in reimbursement can severely impact financial sustainability.
Why First Pass Acceptance Matters
First pass acceptance refers to the rate at which claims are processed and paid by payers without any need for resubmission or further intervention. Increasing this rate has a significant positive effect on both financial operations and overall efficiency. ASCs that prioritize boosting their first pass acceptance rates see improvements in:
- Revenue cycle management: Faster reimbursements lead to healthier cash flow.
- Staff efficiency: With fewer denials to manage, administrative staff can focus on other essential tasks.
- Patient satisfaction: Quicker claims processing leads to a smoother billing experience, enhancing overall patient satisfaction.
A Customer Success Story: Boosting First Pass Acceptance to Improve Financial Health
One ASC that embraced a focus on first pass acceptance saw remarkable results. The center, struggling with frequent claims denials and slow reimbursements, made strategic changes in its claims submission process. By improving their first pass acceptance rate by 15%, the ASC was able to:
- Reduce manual claims intervention by 30%: With fewer denials, staff spent less time on resubmissions.
- Cut reimbursement delays by 25%: This improvement not only stabilized cash flow but also helped the ASC meet financial obligations more quickly.
- Enhance patient satisfaction scores by 10%: Patients appreciated faster and more transparent billing processes, leading to improved satisfaction ratings.
How to Improve First Pass Acceptance Rates
Here are actionable steps ASCs can take to improve their first pass acceptance rates and minimize reimbursement delays:
1. Invest in Claims Scrubbing Technology
Claims scrubbing software automatically reviews claims for common errors before submission, drastically reducing the chances of denial. This technology ensures that claims are accurate and complete, improving the chances of first-pass approval. By catching errors such as incorrect coding or missing patient information, scrubbing software helps ensure that claims are processed correctly the first time.
2. Prioritize Accurate Documentation and Coding
One of the leading causes of denied claims is inaccurate or incomplete documentation. ASCs should ensure that medical coders are well-trained and stay up-to-date on the latest billing codes and payer requirements. Regular audits can help catch recurring errors and improve documentation accuracy across the board.
3. Automate Eligibility Verification
Verifying patient insurance coverage before the procedure is a crucial step in preventing denials. By automating eligibility verification, ASCs can ensure that patients are covered for the procedures they are undergoing, reducing the risk of denied claims for coverage-related issues.
4. Strengthen Communication Between Clinical and Billing Teams
Better communication between clinical and billing teams can streamline the claims process. By ensuring that clinical staff understand the importance of complete and accurate documentation, ASCs can reduce the likelihood of denials based on incomplete medical records. Collaborative workflows between departments also help identify potential claim issues before submission.
5. Leverage Analytics to Identify Trends
Analytics tools can help ASCs identify patterns in claims denials and first-pass failures. By pinpointing the most common reasons for denied claims, ASCs can adjust their processes to address these recurring issues. Regular monitoring and adjustment can help maintain a high first pass acceptance rate and ensure that claims are processed efficiently.
Benefits of Reducing Manual Interventions in Claims Management
When first pass acceptance rates improve, the need for manual interventions in claims management decreases significantly. This reduction in manual work offers several advantages:
- Lower administrative costs: With fewer claims to resubmit or appeal, administrative staff can focus on more strategic tasks.
- Increased staff productivity: Employees spend less time tracking and resubmitting claims, which improves overall operational efficiency.
- Improved morale: Staff are less burdened by the tedious and frustrating process of dealing with denied claims.
Speeding Up Reimbursements to Enhance the Patient Experience
Faster claims processing and reimbursement directly benefit patients as well as the ASC:
- Billing transparency: When reimbursements are processed quickly, patients receive clearer and more accurate billing statements, reducing confusion and improving the overall experience.
- Smoother payment processes: Patients are less likely to experience delays in receiving final bills, which can often cause frustration or stress. A quick, smooth billing process ensures a positive interaction at every touchpoint.
- Higher patient satisfaction: Ultimately, patients appreciate efficiency, especially when it comes to the financial aspects of their care. Improved reimbursement times enhance their experience and can lead to increased patient loyalty.
How HUB Healthcare Can Help
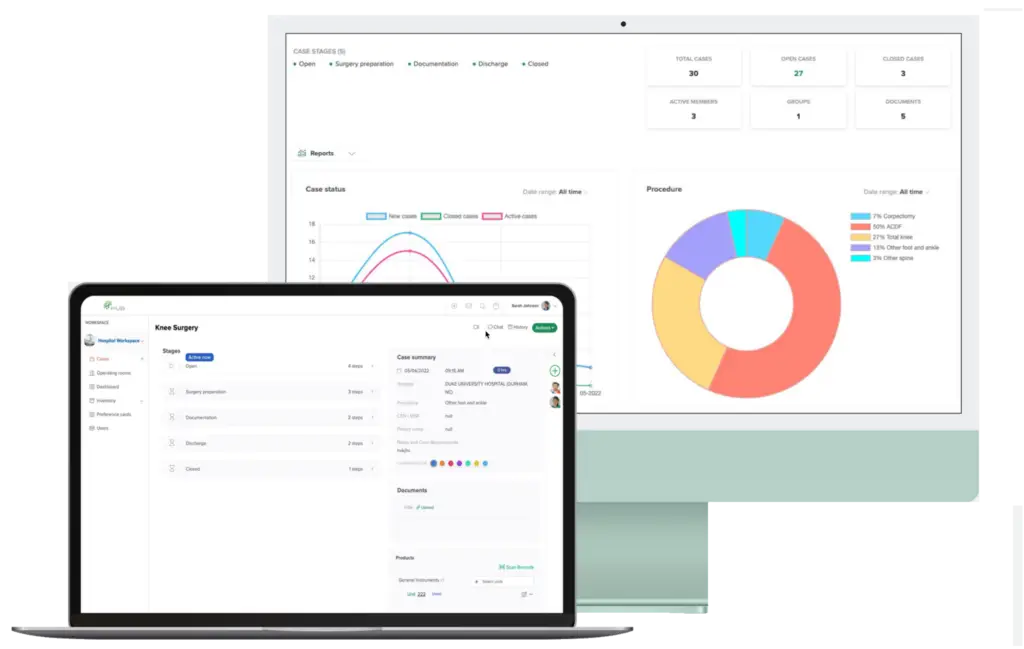
HUB Healthcare offers a comprehensive solution designed to enhance communication in healthcare, streamline care coordination, and improve overall workflow efficiency. Our platform includes features such as medical case management software, healthcare document management, and healthcare analytics to ensure that all aspects of patient care are optimized. By leveraging HUB Healthcare’s robust tools, organizations can reduce workflow bottlenecks, automate repetitive tasks, and facilitate better collaboration among healthcare providers. This not only improves work quality but also enhances patient outcomes, making HUB Healthcare an essential partner in achieving healthcare excellence.
Conclusion
Boosting first pass acceptance rates is a powerful way for ASCs to manage reimbursement delays and maintain financial stability. By investing in the right tools and processes—such as claims scrubbing technology, automated verification, and improved team communication—ASCs can reduce denials, speed up reimbursement, and improve the overall patient experience. This small but significant shift in focus offers lasting benefits that can improve both operational efficiency and patient satisfaction.
To stay competitive and ensure long-term financial success, ASC leaders must prioritize strategies that enhance their first pass acceptance rates and reduce the need for manual claims management. By taking these steps, ASCs can protect their cash flow and create a better overall experience for both their staff and their patients.